Every breath matters, every story deserves to be heard, and every action brings us closer to change.
This September, we're shining a light on pulmonary fibrosis, a devastating lung disease affecting over 70,000 people in the UK. From powerful stories and community events to fundraising challenges, PF Awareness Month 2025 will amplify patient voices and drive real, life-changing progress.
What is pulmonary fibrosis?
You might be told by your medical team you have ‘lung scarring’ or ‘pulmonary fibrosis’. On this page, we talk about pulmonary fibrosis.
The term pulmonary fibrosis describes scar tissue in the lungs.
Pulmonary – refers to the lungs
Fibrosis – refers to scarring
Scar tissue can make it difficult for the lungs to work normally. Some people with interstitial lung disease (ILD) may develop pulmonary fibrosis.
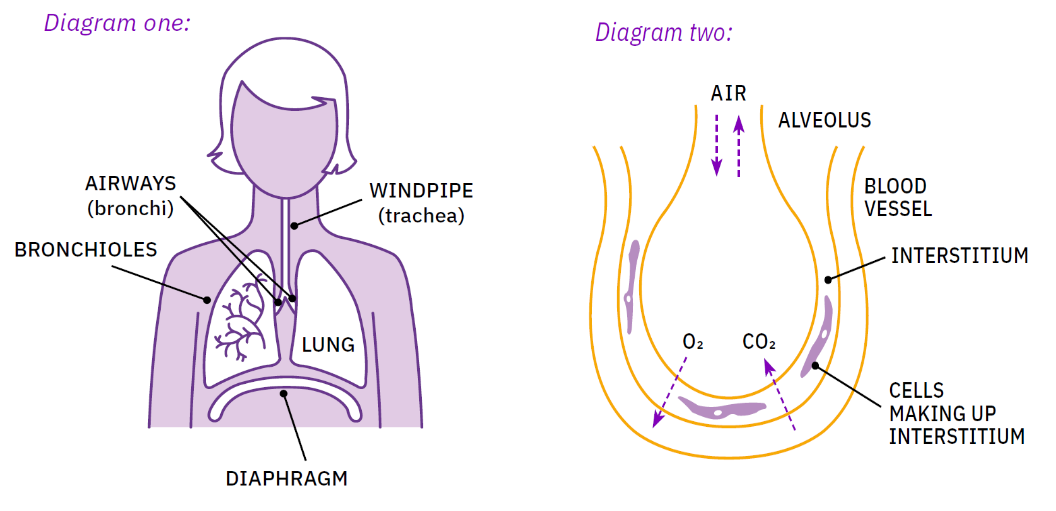
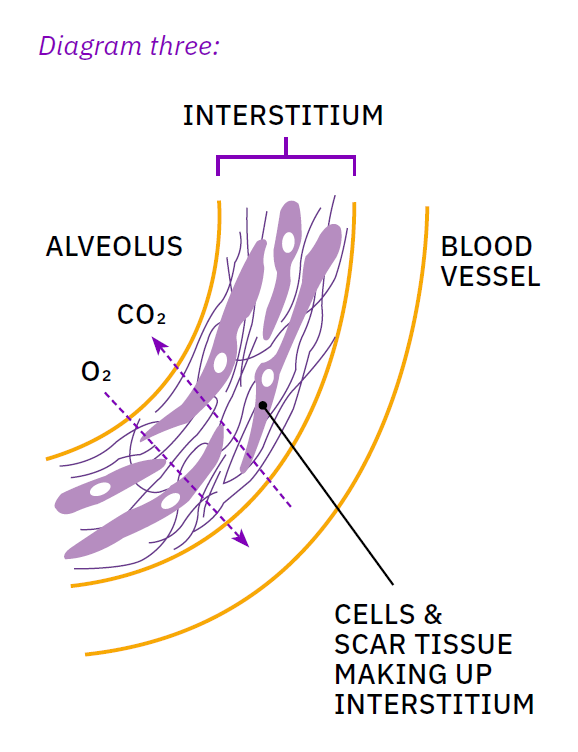
Interstitial lung disease: a group of diseases that affect the interstitium of the lungs. The interstitium is the space in the lungs between the air sacs (alveoli) and the blood vessels. (See diagrams 2 and 3).
How do the lungs work?
Healthy lungs are spongy and stretchy so air can move in and out of them. There’s a network of tubes that carries air through the lungs. At the end of the tubes are small sacs called alveoli, surrounded by blood vessels. Oxygen and carbon dioxide move between the alveoli and the blood. The space between the alveoli and blood vessels is called the interstitium. This space contains different cells that help the lungs work properly.
What happens in the lungs when you have pulmonary fibrosis?
Scar tissue forms in the interstitium and this area becomes thicker. This makes the lungs stiff and less stretchy, which can make you feel short of breath (breathless). Several different mechanisms can cause a cough. Change to the structure of the lungs is one potential cause.
Scar tissue makes it more difficult for oxygen to move between the alveoli and the blood. Because of this, there is less oxygen available for the body to use.
Why does lung scarring happen?
We don’t know exactly what happens in the lungs when someone has pulmonary fibrosis. There’s more research looking into this. From what we have learned so far, two processes can lead to scar tissue in the lungs:
Inflammation
Inflammation is when something causes irritation or injury to the lungs. Some types of ILDs can cause inflammation in the lungs. These ILDs include, but are not limited to, sarcoidosis autoimmune disease-associated ILDs, and hypersensitivity pneumonitis. Inflammation can lead to scar tissue in the lungs (pulmonary fibrosis).
Lung cells age too quickly
Pulmonary fibrosis can happen when cells in the lungs age too quickly.
One of the normal functions of these cells is to repair damage. Ageing lung cells are unable to repair normally. Instead, they cause scar tissue to form. So, factors that cause lung cells to age too quickly increase the risk of pulmonary fibrosis. This includes genes (inherited from your parents), your environment (e.g. dust or smoke that your lungs have breathed in previously), and other risk factors below. Read about risk factors in the next section.
Damage to lung cells is normal. We breathe in over 10,000 litres of air each day. Air may contain dust, pollutants, viruses, bacteria or small amounts of stomach content. These can damage the delicate lining of the lungs. Cells that are lost to damage must be replaced. When a person has pulmonary fibrosis, their body is not able to replace cells as it normally would.
What causes pulmonary fibrosis?
From what we have learned so far, there is no single cause of pulmonary fibrosis. Instead, we talk about different risk factors. Risk factors can lead to inflammation or lung cells ageing too quickly. This can increase the risk of scarring.
Pulmonary fibrosis risk factors
Risk factors for pulmonary fibrosis can include:
- Ageing
- Family history (the genes inherited from your parents)
- Breathing in something that irritates the lungs, such as smoke or dust – this will usually happen repeatedly over a long time
- Some medications
- Other conditions, such as rheumatoid arthritis
- Gastro-oesophageal reflux disease (GORD)
Many people with pulmonary fibrosis have a combination of risk factors. Your medical team will try to find your risk factors. This helps them diagnose the correct type of pulmonary fibrosis.
What are pulmonary fibrosis signs and symptoms?
The signs and symptoms of pulmonary fibrosis vary from person to person. They may also change if the disease progresses.
Pulmonary fibrosis signs
Signs: information that healthcare professionals find.
A common sign is hearing crackles when listening to your breathing with a stethoscope. This sounds similar to Velcro being pulled apart.
Pulmonary fibrosis symptoms
Symptoms: your experience of pulmonary fibrosis.
Common symptoms can include:
- shortness of breath (breathlessness)
- dry cough
- tiredness (fatigue)
- unexplained weight loss
- clubbing of fingers and toes (swollen and rounded finger and toe tips – see diagram four)